On February 5 last year, the Trump administration announced an initiative called Ending the HIV Epidemic: A Plan for America to end the HIV epidemic in the United States by 2030. The plan was developed by the U.S. Department of Health and Human Services (HHS) and sought to reduce the number of HIV infections in the U.S. by 90% in 10-years — meaning 250,000 HIV infections would be avoided.
Phase I of the plan covers the first 5-years, with a goal of 75% of infections being reduced. 57 priority jurisdictions in the U.S. have been identified using data from HIV diagnoses that occurred in 2016 and 2017. These regions include Washington, DC, and San Juan, Puerto Rico, where more than 50 percent of new HIV diagnoses occurred in that time frame. Phase I also targets seven states with a disproportionate occurrence of HIV in rural areas. Each of these jurisdictions will receive a ‘rapid infusion of additional resources, expertise, and technology to develop and implement locally tailored plans.’
Phase II will take a broader approach, with efforts to implement resources across the nation, rather than focusing on specific regions. It is hoped that Phase II will drive down the rate of infection further than the 75% achieved in Phase I, to the goals of 90% reduction in cases by 2030.
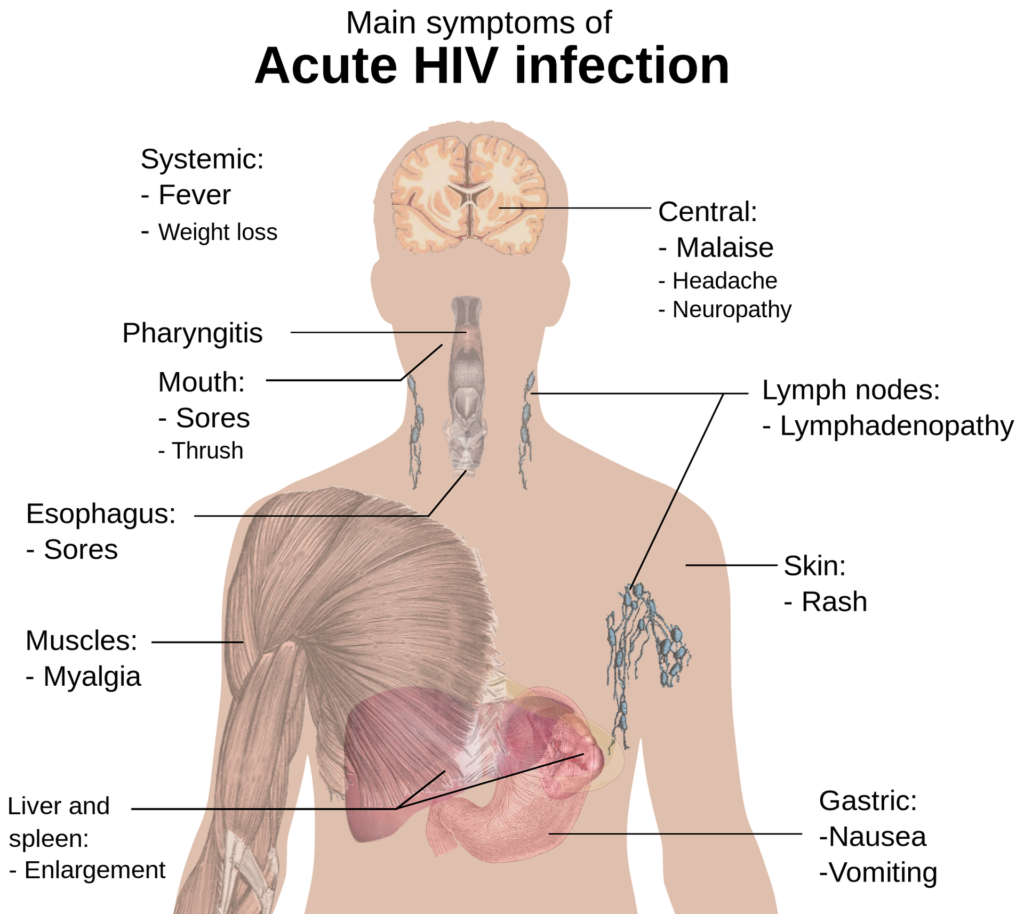
Phase III, is a maintenance period, where ‘intensive case management’ will keep new infections at fewer than 3,000 per year. Currently, there are approximately 40,000 new HIV infections each year, the lowest level on record. While this is an important milestone to have achieved, data shows that the rate of reduction has now plateaued, meaning a new approach is needed to reduce the number of new HIV infections further. CDC data states that in 2016, about 80% of new HIV infections in the U.S. were transmitted by people with HIV who either ‘did not know they had HIV, or who had been diagnosed but were not receiving HIV care.’ The CDC notes that this statistic speaks to the vitality of increasing HIV testing and treatment to increase awareness and minimize further transmission of the virus.
The new plan doesn’t provide specific detail on how it will achieve Phase I, II and III goals. The website notes that the initiative “leverages critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response by coordinating the highly successful programs, resources, and infrastructure of many HHS agencies and offices.” While information on the solution is vague, the new initiative provides significant detail and data on the scope of the epidemic:
- More than 700,000 American lives have been lost to HIV since 1981.
- More than 1.1 million Americans are currently living with HIV and many more are at risk of HIV infection.
- While new HIV diagnoses have declined significantly from their peak, progress on further reducing them has stalled with an estimated 40,000 Americans being newly diagnosed each year. Without intervention another 400,000 Americans will be newly diagnosed over 10 years despite the available tools to prevent transmissions.
- The U.S. government spends $20 billion in annual direct health expenditures for HIV prevention and care.
- There is a real risk of an HIV resurgence due to several factors, including trends in injection drug use; HIV-related stigma; homophobia; lack of access to HIV prevention, testing, and treatment; and a lack of awareness that HIV remains a significant public health threat.
- Thanks to advances in antiretroviral therapy, the medicine used to treat HIV, individuals with HIV who take their medicine as prescribed and, as a result, maintain an undetectable viral load can live long, healthy lives and have effectively no risk of sexually transmitting HIV to a partner.
- We have proven models of effective HIV care and prevention based on more than two decades of experience engaging and retaining patients in effective care.
- Pre-exposure prophylaxis (PrEP), a daily regimen of two oral antiretroviral drugs in a single pill, has proven to be highly effective in preventing HIV infection for individuals at high risk, reducing the risk of acquiring HIV by up to 97 percent.
- New laboratory and epidemiological techniques allow us to pinpoint where HIV infections are spreading most rapidly so health officials can respond swiftly with resources to stop the further spread of new transmissions.
- Not everyone is benefiting equally from advances in treatment. New infections are highly concentrated among men who have sex with men; minorities, especially African Americans, Hispanics/Latinos, and American Indians and Alaska Natives; and those who live in the southern United States.
- Stigma—which can be a debilitating barrier preventing people living with, or at risk for, HIV from receiving the health care, services, and respect they need and deserve—still tragically surrounds HIV. Responding to HIV is not just a biomedical issue, but a social challenge, too.